The Human Heart
Explore the anatomy and core functions of the heart with Innerbody's interactive 3D model.
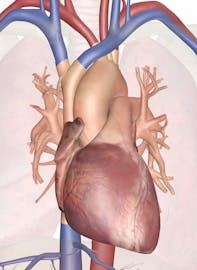
The heart is a muscular organ about the size of a closed fist that functions as the body's circulatory pump. It takes in deoxygenated blood through the veins and delivers it to the lungs for oxygenation before pumping it into the various arteries (which provide oxygen and nutrients to body tissues by transporting the blood throughout the body). The heart is located in the thoracic cavity medial to the lungs and posterior to the sternum.
On its superior end, the base of the heart is attached to the aorta, pulmonary arteries and veins, and the vena cava. The inferior tip of the heart, known as the apex, rests just superior to the diaphragm. The base of the heart is located along the body's midline with the apex pointing toward the left side. Because the heart points to the left, about 2/3 of the heart's mass is found on the left side of the body and the other 1/3 is on the right.
Anatomy of the Heart
Pericardium
The heart sits within a fluid-filled cavity called the pericardial cavity. The walls and lining of the pericardial cavity are a special membrane known as the pericardium. Pericardium is a type of serous membrane that produces serous fluid to lubricate the heart and prevent friction between the ever beating heart and its surrounding organs. Besides lubrication, the pericardium serves to hold the heart in position and maintain a hollow space for the heart to expand into when it is full. The pericardium has 2 layers---a visceral layer that covers the outside of the heart and a parietal layer that forms a sac around the outside of the pericardial cavity.
Structure of the Heart Wall
The heart wall is made of 3 layers: epicardium, myocardium and endocardium.
- Epicardium. The epicardium is the outermost layer of the heart wall and is just another name for the visceral layer of the pericardium. Thus, the epicardium is a thin layer of serous membrane that helps to lubricate and protect the outside of the heart. Below the epicardium is the second, thicker layer of the heart wall: the myocardium.
- Myocardium. The myocardium is the muscular middle layer of the heart wall that contains the cardiac muscle tissue. Myocardium makes up the majority of the thickness and mass of the heart wall and is the part of the heart responsible for pumping blood. Below the myocardium is the thin endocardium layer.
- Endocardium. Endocardium is the simple squamous endothelium layer that lines the inside of the heart. The endocardium is very smooth and is responsible for keeping blood from sticking to the inside of the heart and forming potentially deadly blood clots.
The thickness of the heart wall varies in different parts of the heart. The atria of the heart have a very thin myocardium because they do not need to pump blood very far---only to the nearby ventricles. The ventricles, on the other hand, have a very thick myocardium to pump blood to the lungs or throughout the entire body. The right side of the heart has less myocardium in its walls than the left side because the left side has to pump blood through the entire body while the right side only has to pump to the lungs.
Chambers of the Heart
The heart contains 4 chambers: the right atrium, left atrium, right ventricle, and left ventricle. The atria are smaller than the ventricles and have thinner, less muscular walls than the ventricles. The atria act as receiving chambers for blood, so they are connected to the veins that carry blood to the heart. The ventricles are the larger, stronger pumping chambers that send blood out of the heart. The ventricles are connected to the arteries that carry blood away from the heart.
The chambers on the right side of the heart are smaller and have less myocardium in their heart wall when compared to the left side of the heart. This difference in size between the sides of the heart is related to their functions and the size of the 2 circulatory loops. The right side of the heart maintains pulmonary circulation to the nearby lungs while the left side of the heart pumps blood all the way to the extremities of the body in the systemic circulatory loop.
Valves of the Heart
The heart functions by pumping blood both to the lungs and to the systems of the body. To prevent blood from flowing backwards or "regurgitating" back into the heart, a system of one-way valves are present in the heart. The heart valves can be broken down into two types: atrioventricular and semilunar valves.
- Atrioventricular valves. The atrioventricular (AV) valves are located in the middle of the heart between the atria and ventricles and only allow blood to flow from the atria into the ventricles. The AV valve on the right side of the heart is called the tricuspid valve because it is made of three cusps (flaps) that separate to allow blood to pass through and connect to block regurgitation of blood. The AV valve on the left side of the heart is called the mitral valve or the bicuspid valve because it has two cusps. The AV valves are attached on the ventricular side to tough strings called chordae tendineae. The chordae tendineae pull on the AV valves to keep them from folding backwards and allowing blood to regurgitate past them. During the contraction of the ventricles, the AV valves look like domed parachutes with the chordae tendineae acting as the ropes holding the parachutes taut.
- Semilunar valves. The semilunar valves, so named for the crescent moon shape of their cusps, are located between the ventricles and the arteries that carry blood away from the heart. The semilunar valve on the right side of the heart is the pulmonary valve, so named because it prevents the backflow of blood from the pulmonary trunk into the right ventricle. The semilunar valve on the left side of the heart is the aortic valve, named for the fact that it prevents the aorta from regurgitating blood back into the left ventricle. The semilunar valves are smaller than the AV valves and do not have chordae tendineae to hold them in place. Instead, the cusps of the semilunar valves are cup shaped to catch regurgitating blood and use the blood's pressure to snap shut.
Conduction System of the Heart
The heart is able to both set its own rhythm and to conduct the signals necessary to maintain and coordinate this rhythm throughout its structures. About 1% of the cardiac muscle cells in the heart are responsible for forming the conduction system that sets the pace for the rest of the cardiac muscle cells.
The conduction system starts with the pacemaker of the heart---a small bundle of cells known as the sinoatrial (SA) node. The SA node is located in the wall of the right atrium inferior to the superior vena cava. The SA node is responsible for setting the pace of the heart as a whole and directly signals the atria to contract. The signal from the SA node is picked up by another mass of conductive tissue known as the atrioventricular (AV) node.
The AV node is located in the right atrium in the inferior portion of the interatrial septum. The AV node picks up the signal sent by the SA node and transmits it through the atrioventricular (AV) bundle. The AV bundle is a strand of conductive tissue that runs through the interatrial septum and into the interventricular septum. The AV bundle splits into left and right branches in the interventricular septum and continues running through the septum until they reach the apex of the heart. Branching off from the left and right bundle branches are many Purkinje fibers that carry the signal to the walls of the ventricles, stimulating the cardiac muscle cells to contract in a coordinated manner to efficiently pump blood out of the heart.
Physiology of the Heart
Coronary Systole and Diastole
At any given time the chambers of the heart may found in one of two states:
- Systole. During systole, cardiac muscle tissue is contracting to push blood out of the chamber.
- Diastole. During diastole, the cardiac muscle cells relax to allow the chamber to fill with blood. Blood pressure increases in the major arteries during ventricular systole and decreases during ventricular diastole. This leads to the 2 numbers associated with blood pressure---systolic blood pressure is the higher number and diastolic blood pressure is the lower number. For example, a blood pressure of 120/80 describes the systolic pressure (120) and the diastolic pressure (80).
The Cardiac Cycle
The cardiac cycle includes all of the events that take place during one heartbeat. There are 3 phases to the cardiac cycle: atrial systole, ventricular systole, and relaxation.
- Atrial systole: During the atrial systole phase of the cardiac cycle, the atria contract and push blood into the ventricles. To facilitate this filling, the AV valves stay open and the semilunar valves stay closed to keep arterial blood from re-entering the heart. The atria are much smaller than the ventricles, so they only fill about 25% of the ventricles during this phase. The ventricles remain in diastole during this phase.
- Ventricular systole: During ventricular systole, the ventricles contract to push blood into the aorta and pulmonary trunk. The pressure of the ventricles forces the semilunar valves to open and the AV valves to close. This arrangement of valves allows for blood flow from the ventricles into the arteries. The cardiac muscles of the atria repolarize and enter the state of diastole during this phase.
- Relaxation phase: During the relaxation phase, all 4 chambers of the heart are in diastole as blood pours into the heart from the veins. The ventricles fill to about 75% capacity during this phase and will be completely filled only after the atria enter systole. The cardiac muscle cells of the ventricles repolarize during this phase to prepare for the next round of depolarization and contraction. During this phase, the AV valves open to allow blood to flow freely into the ventricles while the semilunar valves close to prevent the regurgitation of blood from the great arteries into the ventricles.
Blood Flow through the Heart
Deoxygenated blood returning from the body first enters the heart from the superior and inferior vena cava. The blood enters the right atrium and is pumped through the tricuspid valve into the right ventricle. From the right ventricle, the blood is pumped through the pulmonary semilunar valve into the pulmonary trunk.
The pulmonary trunk carries blood to the lungs where it releases carbon dioxide and absorbs oxygen. The blood in the lungs returns to the heart through the pulmonary veins. From the pulmonary veins, blood enters the heart again in the left atrium.
The left atrium contracts to pump blood through the bicuspid (mitral) valve into the left ventricle. The left ventricle pumps blood through the aortic semilunar valve into the aorta. From the aorta, blood enters into systemic circulation throughout the body tissues until it returns to the heart via the vena cava and the cycle repeats.
The Electrocardiogram
The electrocardiogram (also known as an EKG or ECG) is a non-invasive device that measures and monitors the electrical activity of the heart through the skin. The EKG produces a distinctive waveform in response to the electrical changes taking place within the heart.
The first part of the wave, called the P wave, is a small increase in voltage of about 0.1 mV that corresponds to the depolarization of the atria during atrial systole. The next part of the EKG wave is the QRS complex which features a small drop in voltage (Q) a large voltage peak (R) and another small drop in voltage (S). The QRS complex corresponds to the depolarization of the ventricles during ventricular systole. The atria also repolarize during the QRS complex, but have almost no effect on the EKG because they are so much smaller than the ventricles.
The final part of the EKG wave is the T wave, a small peak that follows the QRS complex. The T wave represents the ventricular repolarization during the relaxation phase of the cardiac cycle. Variations in the waveform and distance between the waves of the EKG can be used clinically to diagnose the effects of heart attacks, congenital heart problems, and electrolyte imbalances.
Heart Sounds
The sounds of a normal heartbeat are known as "lubb" and "dupp" and are caused by blood pushing on the valves of the heart. The "lubb" sound comes first in the heartbeat and is the longer of the two heart sounds. The "lubb" sound is produced by the closing of the AV valves at the beginning of ventricular systole. The shorter, sharper "dupp" sound is similarly caused by the closing of the semilunar valves at the end of ventricular systole. During a normal heartbeat, these sounds repeat in a regular pattern of lubb-dupp-pause. Any additional sounds such as liquid rushing or gurgling indicate a structure problem in the heart. The most likely causes of these extraneous sounds are defects in the atrial or ventricular septum or leakage in the valves.
Cardiac Output
Cardiac output (CO) is the volume of blood being pumped by the heart in one minute. The equation used to find cardiac output is: CO = Stroke Volume x Heart Rate
Stroke volume is the amount of blood pumped into the aorta during each ventricular systole, usually measured in milliliters. Heart rate is the number of heartbeats per minute. The average heart can push around 5 to 5.5 liters per minute at rest.
Heart Health Problems
Heart disease is very common, disrupting the normal function of this important organ and often causing death. Visit our Diseases and Conditions section to learn more about common cardiovascular diseases and how we can prevent them. For information about your personal hereditary risks of a variety of conditions involving the heart (such as those arising from hemochromatosis or G6PDD, to name two very common hereditary disorders), learn more about DNA health testing.










